If dentistry were forced to choose a single unsung hero, saliva would win, every time. Yet xerostomia remains one of the most underdiagnosed, undertreated, and underestimated conditions in clinical practice. As we move into 2026, the evidence is increasingly clear: Dry mouth is not a fringe complaint or an “older adult issue.” It is a silent pandemic, and dentistry has not yet recalibrated its response.¹
And here’s the irony we all recognize chairside: We are trained to eliminate saliva. We suction relentlessly to create a dry field—high‑volume evacuation, cotton rolls, dry angles—because clinically, dryness equals control. But for many patients, saliva isn’t a nuisance. It’s gold. And its loss leads to a rapid decline in comfort, function, confidence, and overall quality of life.²
How prevalent is xerostomia—really?
Statistics show chronic xerostomia affects an estimated 10% to 30% of adults, with substantially higher rates among women, older adults, and individuals taking multiple medications.³ In the United States, roughly one in five adults reports persistent symptoms.
From a clinical standpoint, this is likely an underestimation. Reduced salivary flow has become normalized due to mouth breathing, dehydration, stress, sleep disorders, caffeine, cannabis, metabolic medications, and polypharmacy. Patients assume dryness is baseline.
It isn’t.
Saliva, the oral microbiome, and oral-systemic health
Saliva is not simply fluid; it is a regulatory system. It buffers acids, facilitates remineralization, lubricates tissues, supports taste and digestion, and critically, maintains oral microbiome homeostasis.⁴
When salivary quantity or quality is compromised, microbial balance shifts. Protective species decline. Acidogenic and inflammatory organisms thrive. The result is oral dysbiosis—now increasingly linked to systemic inflammatory burden, cardiometabolic disease, gastrointestinal imbalance, and neuroinflammatory conditions.⁵
Xerostomia is therefore not just a comfort issue; it is a microbiome disruption with oral-systemic consequences.
Primary drivers of dry mouth in the modern patient
While autoimmune disease and oncologic therapies remain contributors, the fastest‑growing causes in 2026 include:
- Medication burden (antidepressants, antihypertensives, antihistamines, anticholinergics, sleep aids, and others)⁶
- GLP‑1 and metabolic therapies
- Chronic dehydration and mouth breathing
- Stress‑mediated cortisol dysregulation
- Cannabis, caffeine, alcohol, and nicotine use
Today’s patient presents with layered risk, with xerostomia often being the earliest signal.
First‑line clinical management: Prescription‑based therapies
For patients with known symptoms, prescription‑level intervention should be considered early, not as a last resort.
Prescription‑based remedies include:
- Lipid‑based oral protectants that reduce transepithelial water loss
- Cholinergic agonists to stimulate salivary flow
- Supersaturated mineral rinses to support mucosal integrity and buffering
Lipid‑based protection: Aquoral, the new player on the field
Lipid‑based oral therapies like Aquoral represent a significant evolution in xerostomia management. Unlike traditional water‑based substitutes, which evaporate quickly, lipid‑based formulations create a protective bioadhesive barrier, mimicking natural oral defense mechanisms and providing longer‑lasting relief.⁷
This category is emerging as a critical adjunct for patients who report that conventional products “don’t last” or require constant reapplication. Importantly, lipid‑based therapy works in conjunction with, not instead of, stimulation and behavioral strategies.
Adjunctive management: Lifestyle and behavioral strategies
Once prescription support is established, outcomes improve when paired with:
- Consistent, distributed hydration
- Nasal breathing and humidification
- Elimination of alcohol‑based rinses
- Reduction of acidic and caffeinated beverages
Saliva stimulation strategies
- Xylitol‑containing gums and lozenges
- Organic acid–based sprays
- Sugar‑free citrus lozenges
Over‑the‑counter relief (product categories)
- Moisturizing toothpastes formulated for xerostomia
- Lubricating oral gels
- Cellulose‑ or glycerin‑based sprays
- Adhering oral discs for nighttime use
- Non‑alcoholic dry mouth rinses
These products provide short‑term surface lubrication, but their primary limitation remains durability. Frequent reapplication is often required, which can undermine compliance.⁸
Measuring what matters: Saliva as data
One of the most important advancements heading into 2026 is our ability to measure salivary health objectively. Modern salivary tools, including tests that measure active MMP‑8, inflammatory mediators, flow rate, buffering capacity, and microbial risk, allow clinicians to move beyond symptom‑based care.⁹
These tools enable:
- Earlier risk detection
- Objective tracking of intervention outcomes
- Personalized prevention and treatment
- Improved patient education and engagement
- Stronger oral–systemic health correlations
Saliva is no longer anecdotal. It is actionable data.
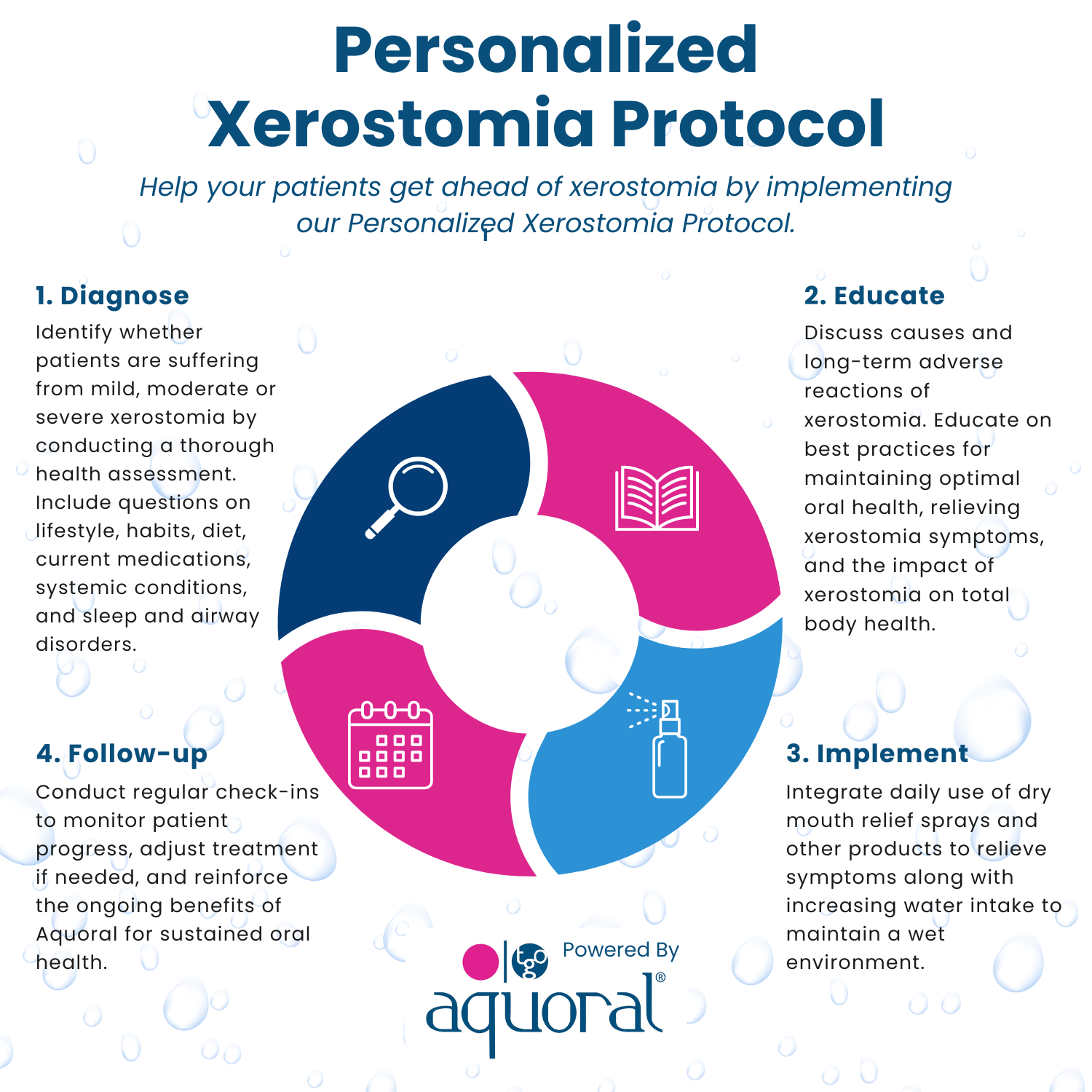
From symptom to system: the Personalized Xerostomia Protocol (PXP)
Structured xerostomia protocols are the future. The Personalized Xerostomia Protocol (PXP) reframes dry mouth as an active, longitudinal care pathway.
PXP supports clinicians in:
- Stratifying risk using health history, medications, airway, sleep, and lifestyle factors
- Educating patients on microbiome and systemic implications
- Implementing individualized relief strategies
- Reassessing and refining care over time
The result is better outcomes, stronger compliance, and increased patient trust.
2026: The year says yes to spit
Dry mouth is not rare. It is not benign. And it is not going away. Stand up to xerostomia. Say yes to spit. Because when saliva fails, everything else follows.
The future of dentistry isn’t just about teeth—it’s about fluids, function, microbiomes, and prevention. And saliva may be the most powerful diagnostic and therapeutic tool we’ve been overlooking all along.
References
- Dawes C. Salivary flow patterns and the health of hard and soft oral tissues. J Am Dent Assoc. 2008.
- Thomson WM. Dry mouth and quality of life. Gerodontology. 2015.
- Villa A, et al. Xerostomia and hyposalivation in the elderly. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015.
- Humphrey SP, Williamson RT. A review of saliva: normal composition, flow, and function. J Prosthet Dent. 2001.
- Farah CS, et al. Oral microbial dysbiosis and systemic disease. Periodontology 2000. 2019.
- Scully C. Drug effects on salivary glands. Oral Dis. 2003.
- Epstein JB, et al. Management of xerostomia. Oral Oncol. 2014.
- Turner MD, Ship JA. Dry mouth and its effects on oral health. J Am Dent Assoc. 2007.
- Alassiri S, et al. Active MMP‑8 as a biomarker in periodontal and systemic disease. Diagnostics. 2020.
About the author
Melissa K. Turner is a dental industry brand strategist, healthcare innovation advisor, and clinical thought leader specializing in saliva, the oral microbiome, and clinical technology. She designs influence systems that shape how innovation earns trust and adoption across dentistry and healthcare. Turner is the co-founder of The Denobi Awards and the National Mobile & Teledentistry Conference, and the creator of the HALO System™ (Human + AI Leadership Optimization). Her work bridges clinical insight, brand strategy, and emerging technology to help organizations and leaders build credibility in an AI-driven world. To become XPERT Certified or receive your free downloadable xerostomia protocol, contact hello@melissakturner.com. Click here to subscribe to Melissa’s new weekly LinkedIn newsletter, The Future of Dentistry Report.
